REDUCING DEATHS AMONG REFUGEE MOTHERS IN ADJUMANI THROUGH MOTIVATING MIDWIVES
By Bazio Doreen.
Each year, an estimated 358,000 women in especially developing countries die while pregnant or giving birth and 2 million newborns die within the first 24 hours of life because of inadequate or insufficient health care. During the COVID-19 pandemic in 2020, each day approximately 800 women died from preventable causes related to pregnancy and childbirth – meaning that a woman died around every two minutes. Observers say these statistics could be lessened if midwifery services are prioritized or upgraded. Uganda has made strides!
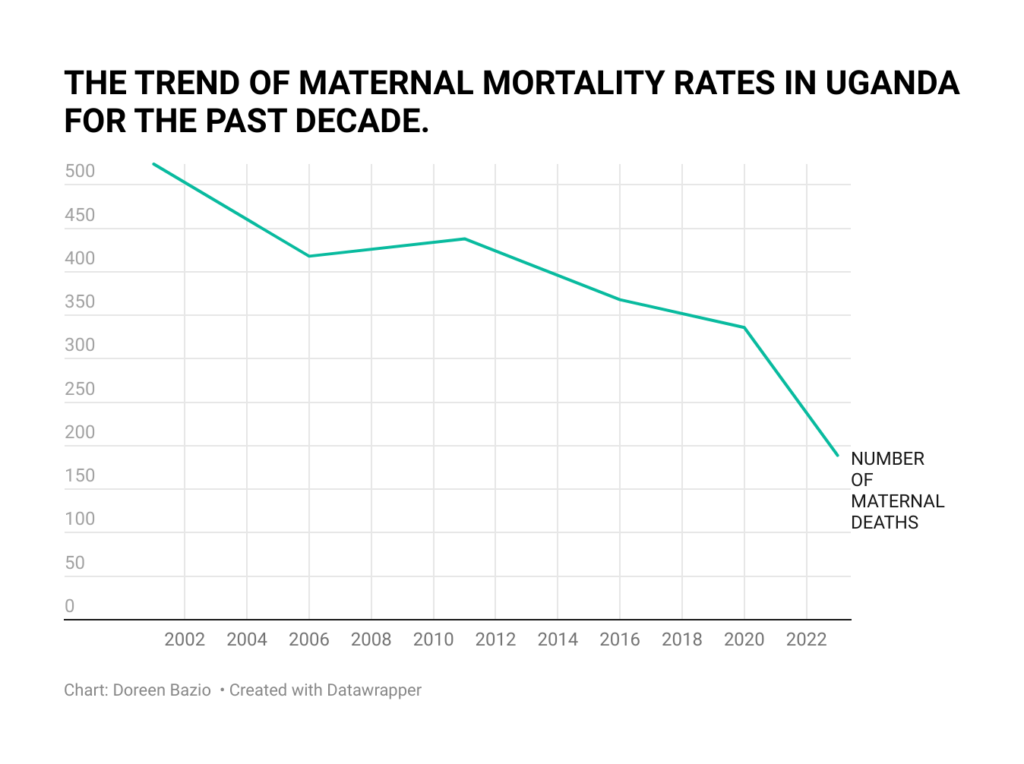
According to the 2022 Uganda Demographic Health Survey, recently (2023) released, maternal morbidity reduced from 524 (2001) to 189 (2022) deaths per 100,000 live births. This is mainly because development partners have joined the government in its effort to improve health service delivery at all levels. This is important because Sustainable Development Goal (SDG) target 3.1 is to reduce maternal mortality to less than 70 maternal deaths per 100,000 live births by 2030.
The situation in Adjumani.
According to Lulu Henry Leku, the Assistant District Health Officer in charge of Maternal Health, among the 36,000 deliveries registered in Adjumani District in the last three financial years (between 2020 and 2023), only 7 maternal deaths occurred. For a refugee-hosting district where resources are usually meager, what has then been the magic cure?
As a patient narrates her experience, you realize that the solution lies in not just ensuring that all that is required is available, but putting in place dedicated staff with a passion for bringing life forth.
For Chandia Stella, a refugee, and mother of three, the experience of labor is always new. There might be some experience but it never means expertise. As fate would have it, Stella and Harriet met in the labor ward as strangers but left as friends.
Harriet Agwang is a midwife recruited by EMESCO Development Foundation, an NGO supporting health service delivery at Agojo HC II, Agojo Refugee Settlement, Ciforo Sub County, in Adjumani District. She has served there for only 10 months as per the project. But in this about a year, Harriet has touched the lives of many.
Difficult moment.
Harriet’s competence was put to the test when in the middle of the night, Stella was due for labor but had complications. But she had more to worry about, there were 5 other mothers in the ward and they all needed her attention. Stella stayed all night trusting that God would come through for her. At least she felt, she was in the best care.
Harriet dozed off and lay beside her waiting and monitoring her progress. Looking back, Stella says she felt sorry that Harriet had to sleep by her side without any mosquito net. She feared that they might survive the battle to bring her son to the world alive but Harriet may have contracted Malaria. But she stayed strong and thanked God that she had met a good nurse on duty on her expected day of delivery.
Regains faith.
Stella had met Harriet before and heard good things about her passion for work, but they had really never been in a difficult situation together for her to experience it. Besides, she believed that that was her routine work and was probably paid to do so. But she was now more impressed about her human side. She could have decided to go and have a rest in her bed as they waited. Hours later, her son was delivered but the complications continued. She had lost her faith but her son won the battle and still continues to live.
Intervention by EMESCO
Stella is one of the 866 women who received pre-natal consultation services and delivery care. These were offered at Alere and Agojo HCIIs through the recruitment of a midwife at each. According to Stella however, Mothers at Agojo HCII just like in many other parts of the district, suffer from many other challenges ranging from the small delivery beds to the lack of reliable ambulance services and unstable electricity supply.
Harriet who also worked during COVID-19 observed that SOPs were greatly hard to manage for mothers and that could partly explain the high numbers of maternal mortality rate at the time. However, the Ugandan government has since learned its lessons and is now doing better.
Future.
For refugees, UNFPA works in partnership with the Ministry of Health to improve delivery care by strengthening health systems; and training health workers, in particular midwives who are then recruited to work in some of the most hard-to-reach parts of the country like Adjumani and other refugee hosting districts.
According to the State Minister in charge of Primary Health Care, Hon. Margaret Muhanga, the Ministry of Health in Uganda has also been able to ensure that 85% of the population has a 5km radius of a health center. The Ministry of Health also established a system that allows them to identify and categorize women at risk, as well as to continuously monitor and ensure their continued care through pregnancy mapping done by the village health teams and volunteers (partners).
Every year, Uganda hosts the ‘Safe Motherhood Conference’ as an opportunity to reflect on the progress made in delivering the different components of safe motherhood and also provide inputs in the key agenda and campaigns focused on improving maternal and reproductive health in the country.
END.
